5 ‘silent symptoms’ of perimenopause you might not be expecting
From not feeling yourself to itchy skin, here's what to look for.
By Emma Thomas, coach and founder of Managing the Menopause
Have you ever thought one or more of the following things, or said it to a partner or friend?
“I used to be able to cope with juggling a million things, what’s wrong all of a sudden?”
“Yesterday I completely missed an important phone call, and today I couldn’t find my car keys. I ended up finding them still in the car ignition. Could I have early-onset dementia?”
“I swear my right hip suddenly hurts every morning when I wake up. Do I have arthritis?”
“My confidence at work has plummeted to zero, there’s no way I could apply for that promotion.”
“I just don’t feel like myself any more.”
If so, then you may be experiencing some of the ‘silent symptoms’ of perimenopause, and you’re not alone.
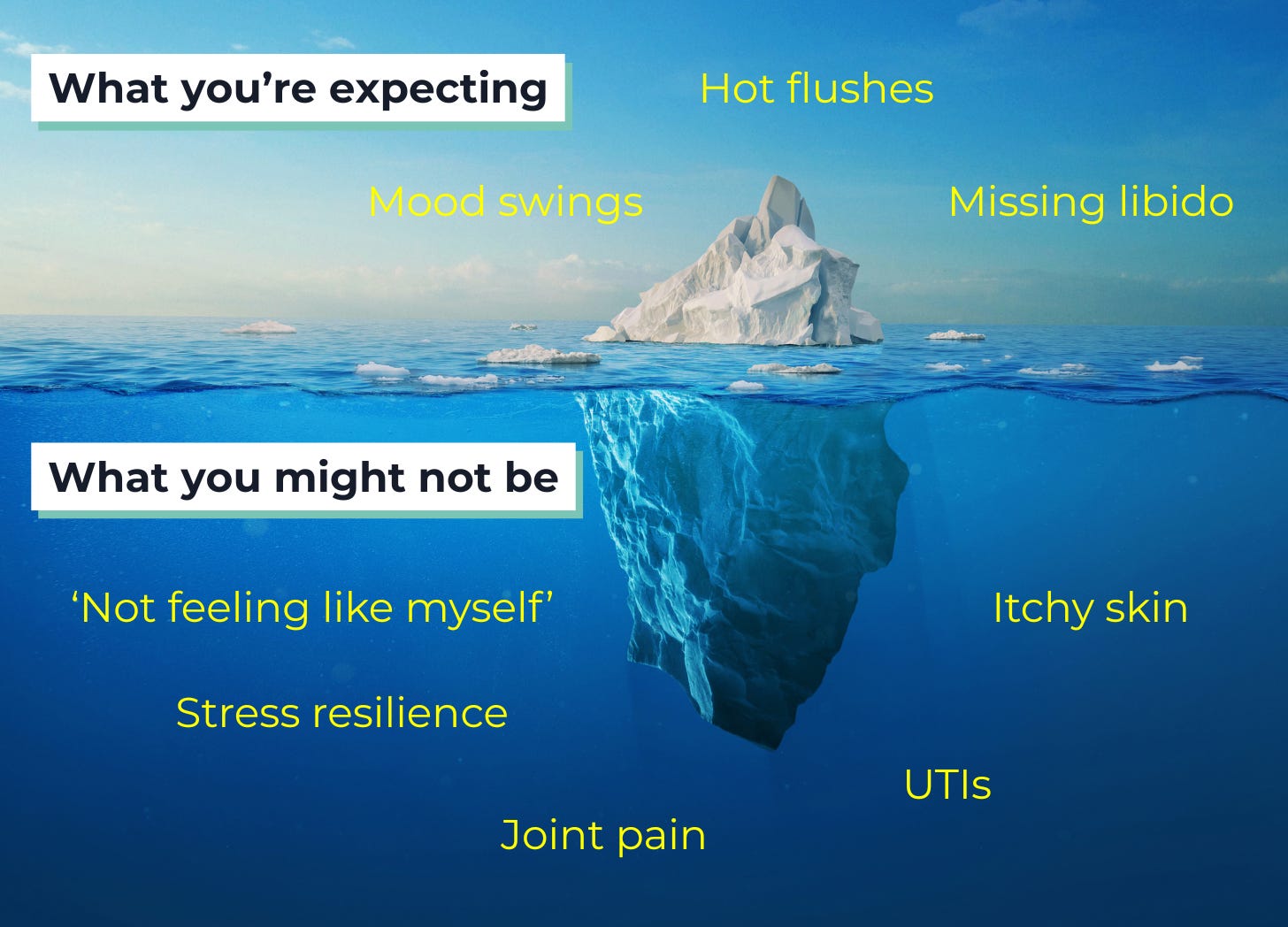
Perimenopause is the time when a woman’s body starts to transition to menopause, and can start anytime from your mid 30s. We have all heard about hot flushes or flashes, a missing libido and mood swings that travel from zero to ballistic in a nanosecond.
But many more perimenopause symptoms are harder to pinpoint, and thus fly under-the-radar for many of us, perhaps until later when those well-known symptoms make themselves known.
Here’s what to know to work out if you are experiencing it:
1. ‘NFLM’
Perhaps one of the most nebulous symptoms is ‘not feeling like myself’ anymore – in fact, it’s so common that there has been research published describing it with the acronym NFLM. It might include anxiety in individuals that have not previously struggled with it, or low mood, lower levels of confidence, or a general feeling of “bleugh” (the technical term for this is ‘anhedonia’ – see this podcast episode for more details of why our hormones create this nosedive in joy levels, and what we can do about it).
This can be extremely difficult to quantify, and as a result, when women seek help from their healthcare provider, they are often prescribed antidepressants. Whilst there is a place for antidepressant use and many find them helpful; low mood, depression and anxiety caused by hormone changes usually respond better to hormone therapy, so it's important to discuss all the options with your healthcare provider.
2. Lower resilience to stress
The hormonal rollercoaster of perimenopause impacts our levels of cortisol, serotonin and dopamine – playing havoc with things like our ability to plan and focus, our motivation, and resilience to stress.
You’re not imagining things, you really are feeling the impact of stress more acutely than you may have been just a year ago. You might find that you ‘fly off the handle’ more easily with family members, or become overwhelmed more often than you used to. You might feel less inclined to socialise in busy groups or with people you don’t know as well.
Having a healthy dose of self-compassion is key here, as is developing your own stress-mitigation toolkit – whatever that looks like for you.
3. Joint pain
Silent symptoms aren’t just psychological. As our oestrogen levels drop, we also become prone to the musculoskeletal syndrome of menopause (70% of women will experience muscular or bone symptoms, and 25% will be disabled by them, through the transition from perimenopause to postmenopause).
This can include things like joint pain. With a maternal history of osteoarthritis, I panicked when my own hip started to hurt regularly every morning and after prolonged periods of sitting at my desk. Soon after starting hormone therapy the pain completely disappeared. Lower levels of oestrogen impact bone health too – if we are not proactively addressing both through exercise and nutrition, then we risk spending our twilight years fragile and dependent on others for our care.
Related articles
4. Skin issues
The drop in oestrogen (and collagen) can also have a pretty big impact on our skin - whether it’s excessively dry and flaky, itchy, or just more sensitive than before.
You may not need to overhaul your whole regime, or buy products specifically marketed at ‘menopausal skin’, but adding in more hydration and potentially going for products that won’t irritate your skin will help. And don’t forget to stay well hydrated - our thirst cues diminish as we age (isn’t getting older fun!)
5. More UTIs
If you find that you’re getting recurrent UTIs, or just getting them more often, that can also be due to the impact of less oestrogen: not only do tissues get thinner and less elastic, your vaginal microbiome changes and that can contribute to increased risk of UTIs. Localised oestrogen can really help, and it can be taken alone or with systemic HRT and is safe for long-term use.
Don’t ignore them…
Perimenopause is a window of opportunity to invest in our health and put ourselves at the top of our long ‘To Do Lists’.
So don’t ignore those silent symptoms. If you’re not sure what’s going on with your body or mind, try tracking for a few months so you can spot the patterns and get some data. And if you’re concerned, take your findings along to your next doctor’s appointment. There’s a symptom checklist and free guide to getting the best out of your appointment on our website.
Emma Thomas is the host of the Middling Along podcast and an executive coach. Her company Managing the Menopause provides training and education around the menopause transition.





Almost every woman I talk to about perimenopause and menopause talk about what I call 'bolting'. That is the desire to walk out the door and just keep going. One woman I know had a packed suitcase in the corner of her room for three years. Doesn't seem to matter how much they love their families. Bolting beckons
What about blood pressure inching up? They were about to put me on bp meds when I started HRT and it went back down!